64 Psychiatric Disorders: Affective Disorders—Bipolar Disorder
Bipolar Disorder
A person with bipolar disorder (BD) experiences phases of clinical depression as described in the previous chapter and, at other times, they experience mania, a state of exhilarating high energy. During this state, they may sleep very little, have difficulty concentrating, and experience pressure of speech: a perceived need to speak very rapidly to get their thoughts out. They might make poor financial or life decisions.
Historically, BD has been called “manic depression.” The estimated prevalence of BD is around 2.5%, but the disease is often misdiagnosed in the clinic as Major Depression Disorder. One reason this happens is that more people are aware of the symptoms of depression, and these symptoms are generally more easily observed. Mania is more difficult to identify, since in mild cases it may be hard to distinguish from a person just “being in a really good mood”.
Diagnosis of Bipolar Disorder
For a diagnosis of BD according to the DSM-V, a mood cycle has to last for a week or more. The word “bipolar” is often misused in pop culture. Frequent changes in mood from happy to sad does not characterize BD. In fact, for a person to be diagnosed with rapid-cycling bipolar disorder, they need to experience four mood transitions annually! BD is usually diagnosed in adolescence and early adulthood. As with depression, there are some genetic factors involved, since a family history of BD is a risk factor. Concordance rates for identical monozygotic twins are estimated to be between 35%-80%. But, environmental influences may be the precipitating factor in the onset of BD.
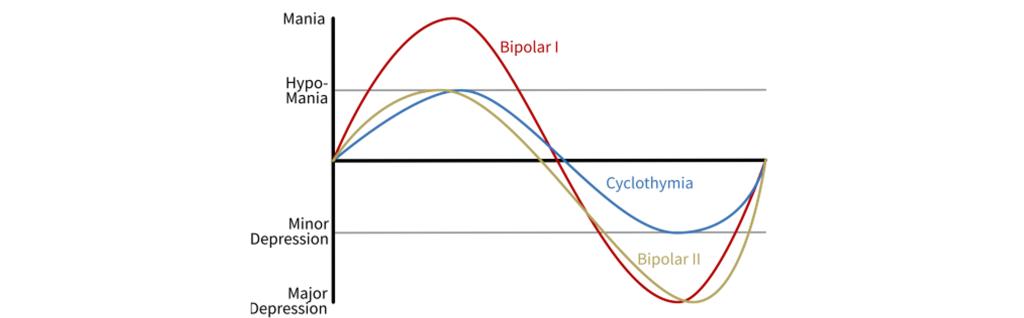
BD is diagnosed into two categories, based roughly on the severity of symptoms. Bipolar 1 disorder is the more severe of the two conditions, with a clinical diagnosis made when a patient experiences depressive or manic events that cause significant social or occupational impairment, or hospitalization to prevent serious self-harm. A diagnosis of Bipolar 2 disorder is less severe, but the behavioral changes are still noticeable by friends and family. A related diagnosis is cyclothymia, where a person has alternating mood states that shift from depression to hypomania, a less severe state of mania. Like most other disorders, BD exists on a spectrum, and these labels only exist for simplicity.
Treatment of Bipolar Disorder
The main issue with BD therapy is bringing the patient to some “middle” state: an antidepressant may treat the depression phase, but could also swing the patient into mania. Similarly, a mania-controlling drug could initiate depression.
Currently, our most reliable therapy for BD is lithium drugs. These compounds are described as mood stabilizers since they act to move the patient’s mood to the center, rather than being at either the high end of mood (mania) or the low end (depression). The way lithium acts to reverse the symptoms is still unknown, and it probably acts on multiple pharmacological targets.
The main downside of this therapy is that lithium is very toxic. It has a very narrow therapeutic window: blood levels of lithium lower than 0.6 mEq/L produce no effect, and anything above 1.5 mEq/L causes delirium, tremor, fatigue, and deadly side effects like seizures and coma. It is also harmful to the kidneys after long exposure. Therefore, a person taking lithium drugs regularly undergo therapeutic drug monitoring, a procedure by which the concentration of lithium is assayed. Therapeutic drug monitoring requires frequent visits to a hospital. Usually, patients get multiple blood draws in the first month when they start lithium treatment, decreasing to one test every 2 months, before decreasing to about four times a year.
Bipolar disorder is very challenging to model in nonhumans. A genetically modified disruption of the circadian rhythm can induce mania-like symptoms, as can extending the length of daytime light exposure; oppositely, decreasing daily light exposure can induce depressive behaviors. Exposure to amphetamine can increase manic behaviors, while withdrawal from the drug can induce depression. Clearly, neither of these models for BD exhibit strong validity.
Key Takeaways
- Bipolar disorder is an affective (mood) disorder.
- Bipolar disorder has periods of both depression and a high energy state, called mania.
- Lithium drugs act as mood stabilizers. Through an unknown mechanism, lithium is effective at treating bipolar disorder, however, lithium is very toxic and patients need to be monitored for toxicity levels.
Attributions
Portions of this chapter were remixed and revised from the following sources:
- Open Neuroscience Initiative by Austin Lim. The original work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Media Attributions
- bipolar disorder © Blacktc adapted by Valerie Hedges is licensed under a CC BY (Attribution) license
state of high energy

